Patient Highlights
- Standard-risk myeloma patient in sCR following autologous stem cell transplant
- Patient entered maintenance protocol but discontinued maintenance due to toxicity
- clonoSEQ Tracking (MRD) Test revealed early signs of relapse 3 years post-transplant
- Clinical relapse observed 6 months after initial MRD-positive clonoSEQ test result
Patient History
- Achieved stringent CR following hyper-CVAD and RVD induction regimen and proceeded to autologous stem cell transplant
- Post-transplant, received 4 cycles of RVD consolidation therapy and began monitoring residual disease via clonoSEQ
- Initiated on lenalidomide maintenance protocol, but developed pancytopenia after one year and discontinued maintenance
- Patient eventually progressed to clinical relapse 2.5 years after maintenance was discontinued
Physician's Perspective
“It’s clear you can say that an MRD-negative result in a low-risk patient bodes well. What you don’t know is if continuing maintenance will change anything. In this case, the patient was standard-risk and wasn’t tolerating maintenance well, I used the MRD-negative clonoSEQ result to justify stopping therapy. I then continued to follow MRD, hoping to use it as an early indicator of relapse. When I saw that first low-level MRD+ result, I wasn’t ready to treat, but I did decide to see him more frequently and the relapse occurred very quickly thereafter.
You never know how fast people are going to progress. The problem is that if someone has a very low MRD level, the disease could progress quickly or it could take a year before it becomes anything. The same is true with a small rise in an M-spike, though. In that case, we might see the patient sooner, get a PET scan sooner, and generally be more vigilant about monitoring to see if the disease is coming back. I use an MRD-positive clonoSEQ result in the same way.”*
*Clinician has received compensation to participate in advisory meetings sponsored by Adaptive. Clinician’s research has also been supported, in part, via product grants.
Use of the clonoSEQ Assay
-

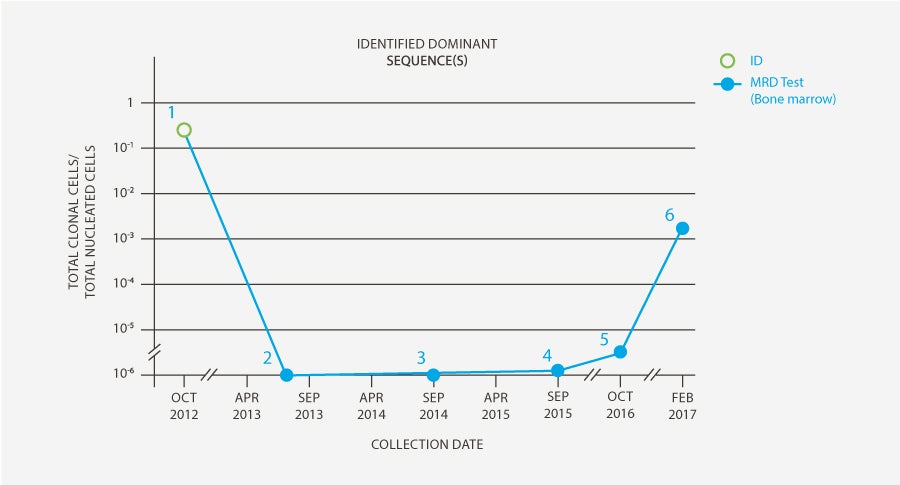
clonoSEQ Clonality (ID) test performed on high-disease load bone marrow sample (collected at diagnosis in October 2012) to identify sequences for subsequent measurable residual disease (MRD) testing.
-

clonoSEQ Tracking (MRD) Test results from a sample collected in July 2013 during post-transplant consolidation therapy found no evidence of residual disease in the bone marrow.
-

clonoSEQ Tracking (MRD) test in September 2014 showed continued MRD-negativity, so maintenance was discontinued and patient’s MRD was tracked using clonoSEQ on an ongoing basis.
-

During routine clonoSEQ testing two years later in August 2016, a low level of residual disease (9 residual cells per million) was detected. Patient was otherwise in sCR.
-

MRD levels continued to rise; the frequency of testing was increased from one year to every six months.
-

Clinical relapse was observed six months after initial MRD-positive clonoSEQ result.
*This case study was based off results generated from an earlier version of the clonoSEQ Assay.
Intended Use:
The clonoSEQ Assay is an in vitro diagnostic that uses multiplex polymerase chain reaction (PCR) and next-generation sequencing (NGS) to identify and quantify rearranged IgH (VDJ), IgH (DJ), IgK and IgL receptor gene sequences, as well as translocated BCL1/IgH (J) and BCL2/IgH (J) sequences in DNA extracted from bone marrow from patients with B-cell acute lymphoblastic leukemia (ALL) or multiple myeloma (MM), and blood or bone marrow from patients with chronic lymphocytic leukemia (CLL).
The clonoSEQ Assay measures minimal residual disease (MRD) to monitor changes in burden of disease during and after treatment. The test is indicated for use by qualified healthcare professionals in accordance with professional guidelines for clinical decision-making and in conjunction with other clinicopathological features.
The clonoSEQ Assay is a single-site assay performed at Adaptive Biotechnologies Corporation in Seattle, Washington.
Special Conditions for Use:
- For in vitro diagnostic use.
- For prescription use only (Rx only).
Limitations:
ALL, MM, and CLL:
MRD values obtained with different assay methods may not be interchangeable due to differences in assay methods and reagent specificity. The results obtained from this assay should always be used in combination with the clinical examination, patient medical history, and other findings. The clonoSEQ Assay is for use with specimens collected in EDTA tubes. Results may vary according to sample time within the course of disease or by sampling site location. The assay may overestimate MRD frequencies near the limit of detection (LoD). The MRD frequency LoD varies based on the amount of gDNA that is tested and using lower gDNA input may prevent MRD detection at low frequencies. Sample processing and cell enrichment strategies may affect the measured MRD frequency. The volume and cellularity of sampled input material may affect the ability to detect low levels of disease. False positive or false negative results may occur for reasons including, but not limited to: contamination; technical and/or biological factors such as the type of rearrangement or the size of the junction region. The assay has been validated with the Illumina NextSeq500 and 550.
For CLL:
MRD is based on measurements of tumor cells detected in peripheral blood and/or bone marrow. However, patients may have significant residual disease in unassessed compartments and U-MRD in one compartment cannot fully rule out the presence of disease in the other compartment, for example, U-MRD in blood may not be the same in bone marrow. Therefore assessment of MRD in CLL should employ a multimodal approach including clinical examination, patient medical history, and other findings. Outcome for patients with MRD detectable in bone marrow but not in peripheral blood (PB-/BM+) may differ according to type of therapy. This assay is capable of monitoring specific tumor clonotypes. The association between MRD assessments and patient clinical status for the purpose of monitoring changes in disease (e.g., relapse, remission, stable disease) has not been demonstrated. The value of MRD in CLL for previously untreated or “watch and wait” patients is not established. CLL is a heterogeneous disease. MRD values and expectations for outcome may not be generalizable across treatments. Changes in MRD should be interpreted with caution when used to evaluate disease burden in therapies that have not been validated. Regardless of MRD status, cytogenetics play an independent role in patient risk status and its impact on PFS/OS.
For important information about the FDA-cleared uses of clonoSEQ including test limitations, please visit clonoSEQ.com/technical-summary.
 Back
Back